The Pandemic Public Health Paradox
A pandemic describes a level of disease burden across significant geography of the whole world. The World Health Organization (WHO) declared that the virus, SARS-CoV-2, which causes COVID19, is pandemic on Weds, March 11, 2020. The majority of US states are in the containment phase of SARS-CoV-2 transmission, which means that testing is the priority and only people who are lab-confirmed through international travel or close contacts are isolated. There are some states like WA, NY, and CA that have sustained community transmission through close contact so mitigation becomes the focus. Close contact is defined as being within ~6ft of an infected person for a prolonged period of time – caring for, living with, visiting, or sharing a waiting area or room with – or being directly coughed on and droplet secretions land on your face or you touch droplets spread on a surface (the virus can survive from a few hours up to a day on hard surfaces).
To slow the spread, public health professionals focus on both containment and mitigation, however, it's best to think about these in layers: 1) individual behaviors and precautions, 2) institutional decisions and practices, and 3) community-based pre-emptive interventions. "Why is everything being canceled, closed, or restricted??" Because, first and foremost, social distancing is about keeping healthy people healthy FIRST.
Mitigation means a regional-level transmission; local residents would have the same exposure risk as the international travelers did. It would not be feasible to identify all of the people with symptoms or all potentially exposed contacts (sorry). The risk would still be considered low if you walked by an infected person or were briefly in the same room if you did not meet the definition of close contact. There are known presumed asymptomatic carriers as well. Testing is not recommended for contacts of contacts, meaning exposure to people with no symptoms with potential exposure to SARS-CoV-2. The day that there is an onset of symptoms, it becomes about the management of the risk through quarantine, active or self-monitoring, controlled travel, immediate isolation, medical evaluation as directed for persons under investigation (the infected person wears the mask in this case), social distancing, and cancellation of long-distance travel on planes, trains, and other public transportation. Once recovered, it is feasible for the person to resume normal activities.
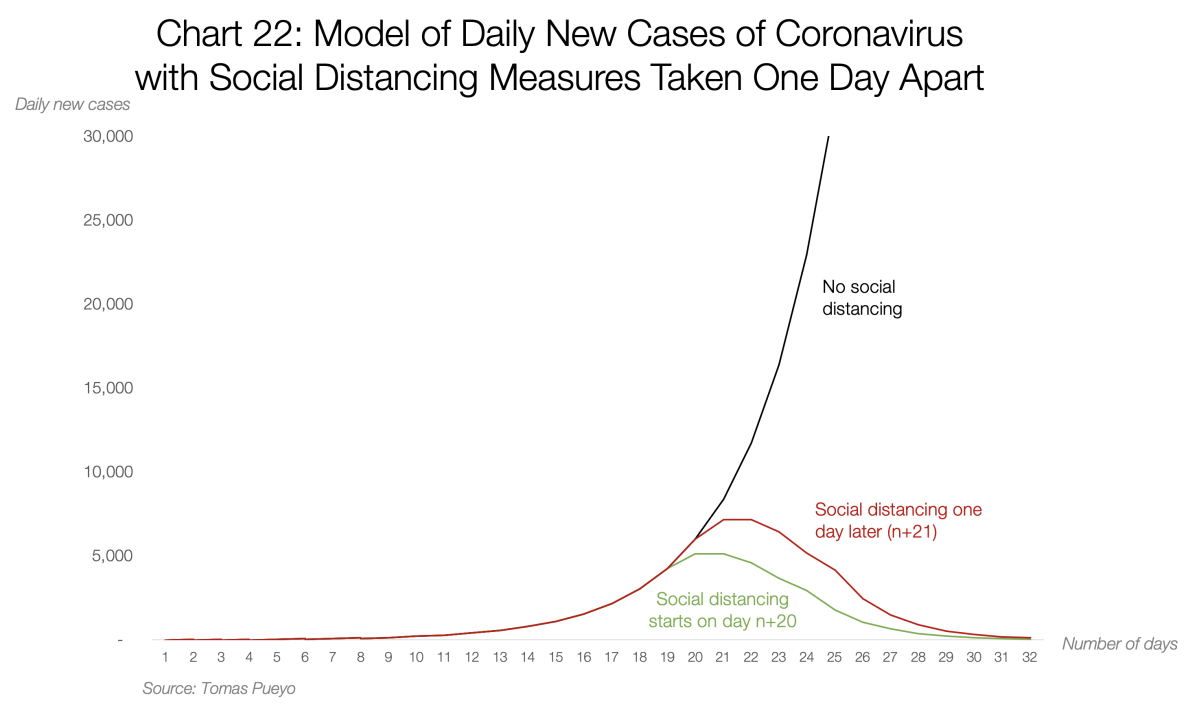
Social distancing can significantly reduce exposure to one another. You can't get sick if you're not exposed - this is the theory behind #flattenthecurve. The eventuality of this being widespread is absolutely still probable--estimates state that upwards of 60% OF Americans will get this novel virus that has no cure or vaccine (yet) and we have no natural immunity to it. And, we are smart enough to work together to slow the spread by social distancing as the prime pre-emptive intervention.
We know that the US has local transmission already. Public health is doing their best with the little they have to conduct surveillance to know the actual burden (significant cuts over the years to public health have hurt our abilities to respond well). Testing is significantly lacking and not happening widely (and effectively) enough, so we can assume the virus spreads unseen. Although we can use the data we do have to help us make decisions: lab-confirmed cases in the US have increased by 204% from March 8 (436) to March 12 (1,323) in four days. (Consult the JHU Dashboard for daily updates.) One Harvard study modeled the spread increasing 10 times every 10 days. My concern is when people struggling to breathe show up en masse to our hospitals, the overburden will stall or halt our health care system and their resources (i.e., Evergreen Hospital in Washington is out of beds, a clear warning sign). Not good. At all.
When prevention efforts work, it often looks like they weren’t needed, and then, because they worked, we have the luxury of thinking exactly that. Public health does our best work when you don’t even know we did anything (that's the paradox). Our systems worked. People remained healthy. All is well. Prevention is always the right decision. We must keep wondering if we should be social distancing and washing our hands so much. Because the moment we’re no longer wondering whether we should be doing it, it’s too late, and that’s a bad place to be. The biggest challenge of social distancing (or working, or doing school, at home) is to not feel that we’re just sitting around waiting in anticipation of developing an inevitable outcome of contracting the coronavirus. It’s NOT inevitable. The steps we are taking are aimed at decreasing the probability, and that’s the best pre-emptive thing we have right now! Remember, this virus has no cure, no vaccine (yet), and we have no immunity to it. Keep healthy people healthy FIRST.
So, this brings me to what if this doesn’t work--all this social distancing and hand hygiene stuff? What if it gets bad and we reach widespread levels of this virus? That’s where community-based mitigation strategies can be implemented! This means things like drive-through testing (go, Denver!), mobile hospitals, enhancement in the number of beds (especially in the ICU), utilization of multiple ventilators, networking among hospitals and HC systems, advanced equipment (and ways to get them quickly), mechanisms to rapidly create temporary isolation facilities, telemedicine practices, preparing the medical reserve corps, systems to restrict access to exposed health care workers, etc. Contingency plans matter and there are task forces and workgroups happening at all levels of local, state, and national public health. This is no different from other pandemic preparedness efforts. We have to promote and support science and pragmatism to plot worst-case scenarios of pandemics vs. available resources at the local level. We have to make sure we are optimizing everything we can with the brief time we have ahead of us. Hopefully, you've begun to hear from your local health departments and/or local governments about their strategies and recommendations.
If all of this hunker-down, stay-home decision-making is hurting your heart, I understand. If your conference or meeting or special vacation was canceled or postponed, I get it. Don't take it personally because you aren't sick or don't know anyone who has COVID19; this isn't about you. Well, it is and it isn't. On things like this, community and public health have to supersede the individual and focus on populations. You may or may not realize it but there are people who are vulnerable, have underlying health conditions, are underresourced, and need help and protection. You may have the means to endure a period of social distancing, but recognize that there are others who don't and public health will need to support them with limited resources. Many cases are recovering, which is awesome news, and part of the equation in reducing the burden of disease within our US population. My health is your health, and your health is my health.
Tap into your altruism and keep perspective on the fact that social distancing is a tremendous act of generosity and solidarity. We do not want to be in the position that Italy is in, and we could easily be within a week or so. Distance is not isolation--keep being kind to each other. Maybe we all need a little slow down in our lives...oh, and, go WASH your hands. Right now.

Project Officer at Health Resources and Services Administration (HRSAgov), HHS
4yVery informative and an excellent reminder as to why #socialdistancing is such an important measure in slowing the spread of #covid19
Network Engineer
4ySharing this!
Well said Dr. Hoglund!