Abstract
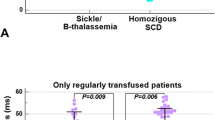
Sickle hepatopathy is a severe and not rare complication of sickle cell disease (SCD), showing mainly a cholestatic pattern. So far, no effective approaches to prevent or treat this condition have been recognized. We conducted a single-center observational study in 68 adult sickle cell patients, encompassing 17 with sickle cell anemia (SCA), 38 with sickle cell thalassemia (HbS/β-Thal), and 13 with HbSC disease. The aim of our study was to assess liver damage in the three main forms of SCD, through the evaluation of clinical, laboratory, and imaging findings. In our population, the role of hepatotropic viruses, high BMI, and alcohol consumption in liver damage was ruled out. SCA and HbS/β-Thal patients with lower Hb (p < 0.001), higher HbS (p < 0.001), and frequent vaso-occlusive crises showed functional (GGT values: SCA and HbS/β-Thal vs HbSC p = 0.047 and p = 0.009, respectively) and structural liver abnormalities, defined by abdominal ultrasound and vibration-controlled transient elastography (liver stiffness values: SCA and HbS/β-Thal vs HbSC p 0.022 and p 0.19, respectively), more severe than HbSC patients. Through univariate and multivariate analyses, male sex, SCA genotype, lower HbF, frequent transfusions, increased GGT values, and abnormal liver ultrasound and stiffness were identified as potentially early markers of sickle hepatopathy.


Similar content being viewed by others
References
Rees DC, Williams TN, Gladwin MT (2010) Sickle-cell disease. Lancet 376:2018–2031
Thein MS et al (2017) Sickle cell disease in older adult. Pathology 49(1):1–9
Banerjee S, Owen C, Chopra S (2001) Sickle cell hepatopathy. Hepatology 35(5):1021–1028
Fraquelli M, Cassinerio E, Roghi A, Rigamonti C, Casazza G, Colombo M, Massironi S, Conte D, Cappellini MD (2010) Transient elastography in the assessment of liver fibrosis in adult thalassaemia patients. Am J Hematol 85:564–568
Drasar E, Fitzpatrick E, Gardner K, et al. (2016) Interim assessment of liver damage in patients with sickle cell disease using new non-invasive techniques. Br J Haematol
Koh C, Turner T, Zhao X, et al. (2013) Liver stiffness increases acutely during sickle cell vaso-occlusive crisis. Am J Hematol 88(11)
Fraquelli M, Rigamonti C, Casazza G et al (2007) Reproducibility of transient elastography in the evaluation of liver fibrosis in patients with chronic liver disease. Gut 56:968–973
Mavrogeni SI, Gotsis ED, Markussis V, Tsekos N, Politis C, Vretou E, Kremastinos D (1998) T2 relaxation time study of iron overload in b-thalassemia. MAGMA 6:7–12
Anderson LJ, Holden S, Davies B et al (2001) Cardiovascular T2* (T2 star) magnetic resonance for the early diagnosis of myocardial iron overload. Eur Heart J 22:2171–2179
Wood JC, Enriquez C, Ghugre N, Tyzka JM, Carson S, Nelson MD, Coates TD (2005) MRI R2 and R2* mapping accurately estimates hepatic iron concentration in transfusion-dependent thalassaemia and sickle cell disease patients. Blood 106:1460–1465
Gardner K, Suddle A, Kane P, O’Grady J, Heaton N, Bomford A, Thein SL (2014) How we treat sickle cell hepatopathy and liver transplantation in adults. Blood 123:2302–2307
Santi L, Montanari G, Bernardi S et al (2009) Liver cirrhosis in a patient with sickle cell trait (Hb Sβ+ thalassaemia) without other known causes of hepatic disease. Case Rep Gastroenterol 3:275–279
Traina S, Gonçalves Jorge S, Yamanaka A et al (2007) Chronic liver abnormalities in sickle cell disease: a Clinicopathological study in 70 living patients. Acta Haematol 118:129–135
Charlotte F, Bachir D, Nénert M, Mavier P, Galactéros F, Dhumeaux D, Zafrani ES (1995 Jan) Vascular lesions of the liver in sickle cell disease. A clinicopathological study in 26 living patients. Arch Pathol Lab Med 119(1):46–52
Colli A, Berzuini A, Prati D (2018) Liver sequestration in sickle-cell disease and hepatitis. Lancet 392:e16
D’Ambrosio R, Maggioni M, Donato MF, Lampertico P, Cappellini MD, Graziadei G (2017) Decompensated cirrhosis and sickle cell disease: case reports and review of the literature. Haemoglobin 41(2):131–133
Pinto VM, Gianesin B, Balocco M et al (2017) Noninvasive monitoring of liver fibrosis in sickle cell disease: longitudinal observation of a cohort of adult patients. Am J Hematol 92(12):E666–E668
Voskaridou E, Schina M, Plata E, Christoulas D, Tsalkani M, Dimopoulou M, Dimitrakopoulou H, Mousoulis G, Terpos E (2010) Liver transient elastography (FibroScan) correlates with liver iron concentratione and reflects liver fibrosis in patients with sickle cell disease. Blood 116:1646
Acknowledgments
The authors are grateful to all patients and nurses of Rare Diseases Center.
Funding
This study was partially supported by the Italian Ministry of Health and Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico [RC_2019].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bortolotti, M., D’Ambrosio, R., Fraquelli, M. et al. Liver damage and sickle cell disease: genotype relationship. Ann Hematol 99, 2065–2072 (2020). https://doi.org/10.1007/s00277-020-04113-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-020-04113-3