The NCAA has released the following guidance documents related to the resocialization of college sports in the wake of the COVID-19 pandemic:
- “Core Principles of Resocialization of Collegiate Sport”(9/25/20)
- “Resocialization of Collegiate Sport: Developing Standards for Practice and Competition” (7/14/20)
- “Resocialization of Collegiate Sport: Action Plan Considerations” (5/28/20)
Each of the above publications was intended to supplement and update the prior publications to reflect most recent emerging data and information available at the time of release. The NCAA has also published and continues to supplement an FAQ document that contains questions/answers pertaining to the publications. As the resocialization publications have been updated, they have rendered certain of the FAQ content outdated. Those outdated portions of the FAQ have been removed from the published version and have been archived to this document solely for purposes of historical reference. This content is no longer consistent with the Association’s published position and should not be relied upon as guidance.
Questions can be directed to the NCAA Sport Science Institute at ssi@ncaa.org.
Original release: July 16, 2020
Updated: August 14, 2020
As indicated below, these materials are intended as a resource for member schools to use in coordination with applicable government and related institutional policies and guidelines, and they remain subject to further revision as available data and information in this space continue to emerge and evolve. The most recent content updates to these materials are indicated with highlighted text within.
This third NCAA publication regarding resocialization of collegiate sport is intended as an update and supplement to the original publication, Core Principles of Resocialization of Collegiate Sport, and the second NCAA publication Resocialization of Collegiate Sport: Action Plan Considerations. The first publication provided guidance for phasing in sports and was consistent with the federal publication Guidelines: Opening Up America Again. The second NCAA publication emphasized personal and institutional considerations related to preventing the spread of COVID-19.
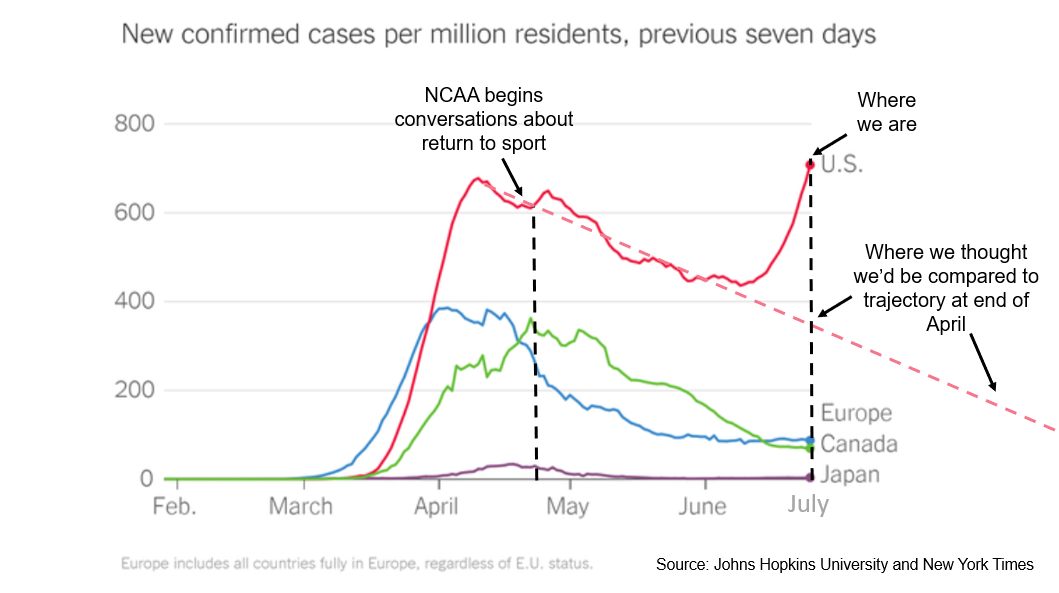
The first two documents were written within the conceptual framework of a national projection for a downward rate of COVID-19 infection in the United States. As the graph below indicates, when the NCAA began discussions about return of sport after the cancellation of 2020 winter and spring championships, there was an expectation that such a return would take place within a context that assumed syndromic surveillance, national testing strategies and enhanced contact tracing. Although testing and contact tracing infrastructure have expanded considerably, the variations in approach to reopening America for business and recreation have correlated with a considerable spike in cases in recent weeks. This requires that schools contemplate a holistic strategy that includes testing to return to sports with a high contact risk.
The information in this third publication was developed in consultation with the NCAA COVID-19 Advisory Panel, the American Medical Society for Sports Medicine (AMSSM) COVID-19 Working Group, which is composed of sports medicine physicians from NCAA member schools who supplement and support the work of the advisory panel as it relates to specific areas of COVID-19 risk: the Autonomy-5 Medical Advisory Group, which includes team physicians and infectious disease experts from the five autonomous conferences; the National Medical Association; the NCAA Committee on Competitive Safeguards and Medical Aspects of Sports. This document also takes into consideration available recommendations from the Centers for Disease Control and Prevention.
These materials are intended to do two things:
- Update and extend the guidance provided in the first two resocialization publications in light of new and emerging information.
- Provide new guidance about considerations specific to the prevention of community spread of COVID-19 in the athletics setting, including, specifically, examples of recommendations for COVID-19 testing for individuals in sports with a high contact risk.
As with prior NCAA publications, the materials are meant to be consistent with guidance published by the federal government and its health agencies. This document reflects the relevant scientific and medical information available at the time of print. These materials should not be used as a substitute for medical or legal advice. Rather, they are intended as a resource for member schools to use in coordination with applicable government and related institutional policies and guidelines, and they remain subject to further revision as available data and information in this space continue to emerge and evolve.
The federal government has not yet published uniform federal guidance related to certain practices like diagnostic testing protocols, contact tracing and surveillance. But as individual states have reopened businesses and entertainment venues, the NCAA COVID-19 Advisory Panel, the AMSSM COVID-19 Working Group, and the Autonomy-5 Medical Advisory Group have reviewed and evaluated those practices. Through this anecdotal evidence and related analysis and discussion, these groups have been able to identify certain practices that should be highlighted for more focused consideration by member schools.
This publication provides NCAA members tools to assist with their efforts to provide a healthy and safe environment for those participating in athletics. While we encourage consideration of various factors and actions, we do not speak to every possible scenario, and in no event should members fall below national or public health standards set by their local communities.
Risk of Transmission of COVID-19
As reported by the CDC, while surface contact may be a risk, the most impactful determinant of COVID-19 spread is human-to-human contact.[1] COVID-19 spread is greatest when individuals are in a crowded environment with prolonged close contact. Further, the risk of COVID-19 transmission is greater in indoor areas with poor ventilation. Indoor areas with good ventilation are better, and outdoor areas are best. Thus, COVID-19 spread is most likely when individuals are in prolonged close contact in an indoor area with poor ventilation, which has implications for both sport training and sport competition planning.[2]
The CDC defines high risk of COVID-19 transmission as any situation in which there has been greater than 15 minutes of close contact, defined as being less than 6 feet apart, with an infectious individual.[3] Importantly, there is a risk of transmission from being present with infectious individuals who are symptomatic, pre-symptomatic or asymptomatic.
Asymptomatic spread of COVID-19 is of significant concern in the college sport environment because, like the broader student body, it is largely composed of younger adults (18-29 years of age). These individuals will often remain asymptomatic after being infected with SARS-CoV-2, but even though they have no symptoms, they are still capable of spreading this virus, which causes COVID-19. If they infect another younger adult, the risk of an adverse outcome is low, although the long-term consequences to cardiopulmonary health to themselves or other younger adults remain unknown. In contrast, contact with that same asymptomatic/minimally symptomatic individual presents a potentially lethal risk for high-risk category individuals who are far more likely to have an adverse outcome if infected with the coronavirus that causes COVID-19. Relatedly, pre-symptomatic spread is also a concern, as these individuals are infected with COVID-19 but have not yet developed symptoms or signs of this disease.
The CDC recently updated its guidance to emphasize that, among adults, the risk for severe illness from COVID-19 increases with age, with older adults at highest risk and 8 out of 10 COVID-19-related deaths reported in the United States to date occurring in adults age 65 and older. In addition, the CDC also has established that individuals of any age with the following underlying medical conditions are at increased risk: [4]
Finally, the CDC has advised that children who have complex medical situations, who have congenital heart disease or who have neurologic, genetic, metabolic conditions are at higher risk for severe illness from COVID-19 than other children.
While data is still fairly limited, the CDC has said people with the following conditions might also be at an increased risk for severe illness from COVID-19:[5]
As published data confirms that the risk of death from COVID-19 increases with age and high-risk underlying medical conditions, students and student-athletes who are not in high-risk categories themselves may be unlikely to have complications from COVID-19, but they represent a significant threat to any high-risk category individuals with whom they may have unprotected contact. These risks must be considered as part of the risk/benefit ratio of resocialization of collegiate sport. Of note, sports such as football may have an overrepresentation of student-athletes (for example, football linemen) who meet the high-risk criteria as it relates to obesity. For this reason, prevention and testing strategies should recognize that some athletes may have an increased risk of adverse outcomes from COVID-19.
Mitigating Risk With Daily Self-Health Checks
Every student-athlete and all athletics personnel should practice at least daily self-health evaluations before participating in any aspect of in-person athletics activities. Individuals who identify any of the following symptoms or signs during the daily self-health evaluation should be encouraged to contact the designated athletics health care representative by telephone or virtual visit before coming on campus or to any athletics facility:
- Shortness of breath or difficulty breathing.
- Cough or other respiratory symptoms.
- Headache.
- Chills.
- Muscle aches.
- Sore throat.
- Congestion or runny nose.
- New loss of taste or smell.
- Nausea, vomiting or diarrhea.
- Pain, redness, swelling or rash on toes or fingers (COVID toes).
- New rash or other skin symptoms.
- High-risk exposure: a new contact with an infected individual or prolonged contact with a crowd without physical distancing (for example, attended a party in which there was no masking or physical distancing).
- Temperature of 100.4° Fahrenheit or above.
Mitigating Risk With Face Coverings and Physical Distancing
Emerging data makes it clear that along with hand washing and good sanitization practices, physical distancing and universal masking are the most effective strategies for preventing COVID-19 spread at the community level. While the CDC continues to recommend wearing “cloth face coverings” in public settings where other social distancing measures are difficult to maintain, some health experts believe it is reasonable to conclude that face shields may be an effective alternative.[6] The use of a face shield, an emerging consideration as either an alternative or supplement to a face mask/cloth face covering, similarly may mitigate spread of virus from an infected individual to a non-infected person. The CDC does not currently recommend that the face shield may replace a cloth face covering, but does note that individuals may choose to use a face shield when sustained close contact with other people is expected, provided the shield wraps around the sides of the wearer’s face and extends to below the chin if used without a mask/cloth face covering.[7] Thus, even where state and local requirements may permit otherwise, schools should consider the recognizable benefit of requiring face coverings and appropriate physical distancing wherever possible in the college athletics environment.
In sport, universal masking would mean that all individuals engaged in athletics activities would wear a mask/cloth face covering during all phases of non-water-based activity that involve proximity to other individuals. This practice could present a challenge during activities involving contact to the head or face region or strenuous exercise. Where a mask/cloth face covering cannot be safely tolerated, schools should consider implementing physical distancing protocols that encourage at least 6 feet between individuals. Schools may want to consider the effectiveness of face shields as a potential alternative to the use of masks/cloth face coverings for protection of others against exposure by asymptomatic individuals. Because face shields are usually made from clear plastic and they generally extend below the chin and around the ears, they may offer some protection but with less impediment in terms of heat, moisture and effective communication. They also have the added benefit of preventing wearers from touching their face.
Face shields also have been developed for football helmets and are made to affix to the helmet’s rigid face mask. Like masks/cloth face covering, the shields are designed to prevent the outward projection of respiratory droplets during coughing, sneezing, heavy breathing, or grunting. It should be noted that these products are considered helmet add-ons and require confirmation from the helmet manufacturer that the helmet can retain necessary National Operating Committee on Standards for Athletic Equipment certification when the shield is added. Schools are advised to confirm with the manufacturer of their football helmets before deciding to purchase or add a face shield product.
Theoretically, if a team can successfully implement universal masking and distancing practices during athletically related activities, it could reduce the risk of spread in the event of an infected team member. Individuals who participate in athletics activities while in proximity (less than 6 feet) to an infected individual and who may otherwise be considered a high-risk contact because of that proximity, could possibly not be considered a high-risk contact for contact tracing purposes if the infected individual was wearing a mask/cloth face covering during those athletics activities. In other words, in addition to lowering the risk of transmission, universal masking practices may potentially ease the operational burden that would otherwise accompany managing a community or team outbreak. This theoretical consideration is likely to be in flux as we understand better the operational considerations for “prolonged exposure” and “close contact in sport.”
Mitigating Risk With Outdoor Training
There is good evidence[2] that risk of COVID-19 transmission is greater in indoor areas with poor ventilation. Indoor areas with good ventilation are better, and outdoor areas are best. This means, to the extent possible, there should be maximization of outdoor activity during training as a strategy to mitigate COVID-19 risk.
When outdoor training is not feasible, or for indoor sports, it is important to try to ensure that ventilation systems are operating properly, air flow is maximized, and physical distancing is maintained. Consider the following CDC recommendations:[2]
- Ensure proper maintenance of ventilation systems.[8]
- Increase circulation of outdoor air as much as possible by opening windows and doors, using fans and following other related methods if doing so does not create a hazard.
- Install transparent shields or other physical barriers in common areas of training where physical distancing may be compromised.
- Use signs, tape marks or other visual cues placed 6 feet apart to encourage physical distancing in common training areas.
- Increase the percentage of outdoor air in HVAC systems.
- Increase total airflow supply to occupied spaces.
- Disable demand-control ventilation controls that reduce air supply based on temperature or occupancy.
- Improve central air filtration.
- Consider running the building ventilation system even during unoccupied times to maximize dilution ventilation.
- Generate clean-to-less-clean air movement.
- Consider using portable high-efficiency particulate air fan/filtration systems to help enhance air cleaning, especially in higher risk areas.
- Ensure exhaust fans in restroom facilities are functional and operating at full capacity when the building is occupied.
- Consider using ultraviolet germicidal irradiation as a supplement to help inactivate the coronavirus.
Impact of State and Institutional Guidelines on Early Resocialization Guidance
As states have evaluated regional risks as they relate to emerging data such as COVID-19 infection and death rates and available medical resources, they have established their own reopening (or resocialization) guidelines. The variations in these resocialization practices and requirements between states are often significant. In addition to this lack of consistency between states, many of the state-level practices are inconsistent with the Guidelines: Opening Up America Again, the federal publication upon which the original Core Principles of Resocialization of Collegiate Sport was based.
For example, many states have elected to forgo strict adherence with the two-week phased intervals of resocialization that were described in the federal Guidelines and Core Principles document and, instead, implemented strategies and practices that emphasize long-term adherence to more practical strategies that mitigate and minimize campus and community spread.
Similarly, the size of the group or gathering has become less of a focus in these state-level strategies as emerging data has suggested that even a very small group can pose a substantial risk if none of the individuals in that group practices risk mitigation strategies (for example, masking and physical distancing). Conversely, if large groups are assembled and effective risk mitigation strategies are in place, such gatherings are consistent with promoting health behaviors that reduce COVID-19 spread.[9] Therefore, the six-week phased-in resocialization approach originally presented in the Core Principles document should now be interpreted and applied in a way that takes into account this emerging data and emphasizes risk mitigation strategies for all groups, regardless of size.
It remains that the first two weeks of return to campus deserve special consideration because student-athletes are converging from multiple parts of the country and may well be asymptomatic, pre-symptomatic, or symptomatic carriers of COVID-19. As athletics departments continue to develop protocols related to student-athlete re-entry to campus, including testing athletes upon campus return, the following considerations identified in the Action Plan document remain relevant, and may warrant consideration of additional testing based on the athlete’s timeline:
- Confirmation of no high-risk exposure to COVID-19 for at least two weeks before returning to campus.
- Absence of typical COVID-19 symptoms.
- Assessment of risk factors involved in traveling back to school.
- Management of infected individuals in accordance with local public health guidance.
Strategies for Transition Periods and Return to Activity
As member schools plan for a return to organized activity for fall sports, questions have emerged about the structure of activity during identified transition and acclimatization periods. COVID-19 has undoubtedly increased the complexities and will continue to impact health and safety considerations related to returning to athletics and preseason activities. Traditional transition and acclimatization considerations (for example, cardiovascular conditioning, heat, altitude) are still very relevant, and when coupled with the loss of spring and summer activities and other physical and nonphysical impacts related to COVID-19, they can create complex re-entry challenges for student-athletes.
Recommendation No. 3 of the NCAA’s Interassociation Recommendations: Preventing Catastrophic Injury and Death in Collegiate Athletes (Catastrophic Materials) speaks to the vulnerability of student-athletes during the first week of activity of a transition period in training and the importance of establishing a seven- to 10-day initial transition period during which student-athletes are afforded the time to properly progress through the physiologic and environmental stresses placed upon them as they return to required activities.
In addition to the NCAA guidance that can be found on the NCAA Coronavirus Resource Page, various evidence-based resources have been published by professional organizations in sports medicine and strength and conditioning. These resources may help inform member schools as they design and implement evaluation activities, physical conditioning and practice sessions during these transition periods impacted by COVID-19. Schools are encouraged to leverage all available resources and information as they plan for return to campus and athletics activities. A nonexhaustive list of some of these materials is included for reference:
Strategies for Resuming Activities After Positive Test Results – Asymptomatic Individuals
The CDC has published strategies for the resumption of normal activities for people who have tested positive for COVID-19 but who have not had any symptoms.[10] Any decision to discontinue isolation of infected individuals should be made in the context of local circumstances.
Symptom-based strategy
For individuals who test positive but never develop symptoms, isolation and other precautions can be discontinued 10 days after the date of their first positive PCR test for SARS-CoV-2.
Strategies for Resuming Activities After Positive Test Results – Symptomatic Individuals
The CDC has published strategies for the resumption of normal activities for people who have tested positive for COVID-19 and who have symptoms.[10] Any decision to discontinue isolation of infected individuals should be made in the context of local circumstances.
Symptom-based strategy
For most people with COVID-19 illness, isolation and precautions can generally be discontinued 10 days after symptom onset and resolution of fever for at least 24 hours, without the use of fever-reducing medications, and with improvement of other symptoms.
A limited number of people with severe illness may warrant extending duration of isolation and precautions for up to 20 days after symptom onset; consultation with infection control experts should be considered.
For people who are severely immunocompromised, a test-based strategy could be considered in consultation with infectious diseases experts, but for all others, a test- based strategy is no longer recommended except if considering discontinuation of isolation other than as outlined above.
Other Considerations Related to Resumption of Activities After Positive Tests
The CDC has identified other information that athletics departments should consider as part of their development of protocols related to the discontinuation of isolation for infected individuals after positive test results.10 For example, for certain populations, including those containing individuals with conditions that may weaken their immune system, a longer isolation timeframe for infected individuals may be desired to minimize the chance of prolonged shedding of the virus. Similarly, it should be noted that recommendations for discontinuing isolation in people known to be infected with COVID-19 may be different than CDC recommendations on when to discontinue quarantine for people known to have been exposed to COVID-19. For example, the CDC still recommends 14 days of quarantine after high-risk exposure based on the time it takes to develop illness if infected. Thus, it is possible that a person known to be infected, but who has been tested, could leave isolation earlier than a person who is quarantined, but who has not been tested, because the possibility of infection remains where testing has not occurred.
Cardiac and Exercise Considerations for Resumption of Exercise After COVID-19 Infection
The COVID-19 virus can potentially negatively impact any endothelial structure, including the heart and lungs, thereby posing a potential risk to individuals who return to exercise post-infection. Published data suggests that athletes with prior COVID-19 infection should undergo cardiac screening.[11],[12] However, it should be noted that the data referenced in these publications was gathered from individuals who suffered severe complications from COVID-19. These individuals did not show the clinical case presentation typical to younger adults who contract the disease and infrequently develop severe complications. To date, there have not been any evidence-based recommendations published to guide the return to exercise in asymptomatic or minimally symptomatic athletes who have become infected with COVID-19.
However, a group of experts from the American Medical Society for Sports Medicine and the American College of Cardiology have developed the following considerations, which are available on the AMSSM website. These recommendations for cardiac testing are based on expert consensus with limited evidence.
Prior Infection
Athletes with a confirmed past infection (antibody or prior diagnostic test), and mild to moderate illness or asymptomatic, (i.e., managed at home):
- A medical evaluation or routine pre-participation exam can be performed, including a symptom screen.
- Electrocardiogramand echocardiogramcan be considered.
- Further workup as indicatedin conjunction with a cardiologist.
Athletes with a confirmed past infection and severe illness (hospitalization) or ongoing cardiovascular symptoms(>14 days from onset of symptoms):
- Medical evaluation with symptom screen.
- Additional testing, which may include:
- Cardiologyconsultation, electrocardiogram; blood troponin 48 hours after exercise and echocardiogram.
- Consider additional cardiac tests such as cardiac MRI, Holter, stress test, chest X-ray, spirometry, pulmonary function tests, d-dimer and chest CT.
New Infection
Athletes with new infection and either no symptoms or mild illness:
- No exercise for at least 10 days, or longer if symptoms persist.
- Monitor for development of symptoms during isolation.
- Cardiac recommendations as above,including consideration of echocardiogram for asymptomatic and mild illness.
- Further work-up as indicated in conjunction with a cardiologist.
Athletes with new infection and mild illness (common cold-like symptoms without fever):
- No exercise for at least 10 days, or longer if symptoms persist.
- Monitor for symptom development with exercise.
- Cardiac recommendations as above,including consideration of echocardiogram for asymptomatic and mild illness.
- Further work-up as indicated in conjunction with a cardiologist.
Athletes with new infection and moderate illness (fever and flu-like illness):
- No exercise for at least 14 days, or longer if symptoms persist.
- Monitor for symptom development with exercise.
- Cardiac recommendations as above.
- Further work-up as indicated in conjunction with a cardiologist.
Athletes with new infection and severe illness (hospitalized):
- For more severe illness, hospitalization, or ongoingcardiovascular symptoms, a comprehensive medical evaluation and cardiologyconsultationis recommended.
- Consider cardiac MRI.
Athletes placed in quarantine for high risk contact but who are not infected with COVID-19:
- Exercise in quarantine is permitted if such exercise does not cause cardiopulmonary symptoms.
- Monitor for development of symptoms during quarantine.
- If symptoms develop, with or without exercise, test for SARS-CoV-2.
Updated Strength and Conditioning Considerations
Because of the number of respiratory droplets that are distributed into the air during a typical strength and conditioning work-out, athletics departments should consider the potential risk mitigation benefits of implementing clear physical distancing and masking practices during such sessions, and such sessions preferably should occur outdoors. See also “Mitigating Risk With Outdoor Training” above. These risks and benefits would apply to athletes and coaches (including strength and conditioning specialists), as well as any other essential personnel involved in these workouts or located within the workout space. See also “Mitigating Risk With Face Coverings and Physical Distancing” above.
Updated Team Practice Considerations
Available data supports the idea that, although sport has many positive effects, group practice activities have the potential to significantly increase the risk of COVID-19 spread if proper distancing and/or masking practices are not implemented, and if air flow/ventilation is compromised. As athletics departments account for and plan to address these risks they should consider the following:
- Face Coverings During Team Practice Activities. See “Mitigating Risk With Face Coverings and Physical Distancing” above.
- Working in Functional Units. Schools should consider the establishment of “functional units” as a strategy to minimize the potential spread of COVID-19. A functional unit may be composed of five to 10 individuals, all members of the same team, who consistently work out and participate in activities together. Assuming that these individuals observe appropriate sanitization, physical distancing and universal masking practices at all other times and do not otherwise place themselves in high contact risk scenarios (for example, attending off-campus social events), the individuals would only be considered high risk to one another. A similar strategy is to have one unit of a team always train against another unit of a team. For example, the first unit of the football team always training against the third unit of the football team; and the second and fourth units always training together. This means that if an individual from one of those units does become infected, the entire team may not be impacted, and contact tracing may be more manageable than it would be otherwise in the event of an infection.
- Electronic Whistles. Schools should consider the use of electronic whistles in practice scenarios as a strategy to avoid the deep breath and forced burst of droplet-filled air that results from the use of a traditional whistle.
Impact of Activities Outside of Athletics
Student-athletes are students first and, although they may be under relatively strict supervision during their daily commitments to athletics, it is likely that little supervision exists during their remaining hours (for example, in the dorms, at the dining facilities, at parties). For this reason, campus policies coupled with a commitment from each student-athlete to practice infection control are integral to the successful mitigation of the risk of COVID-19 spread within and outside of the athletics department. Without the broader campus policies and practices to guide their behavior when away from athletics, student-athletes may incur more risk through their everyday activities than they might as a participant in a sport with high contact risk. Before assuming that the implementation of sanitization, distancing and masking practices are an effective strategy for mitigating risks within the athletics setting, a school should consider whether and to what extent those mitigation practices are successfully occurring outside of athletics activities and whether/how testing protocols may provide an effective supplement to those practices.
Updates Regarding Testing Methodologies
The polymerase chain reaction test, by way of a nasopharyngeal swab, with testing for amplification of the nucleic acid of the SARS-CoV-2 virus, is currently considered the gold standard and has a very high sensitivity and specificity. However, testing paradigms are still rapidly changing, and other strategies may become available. For example, rapidly emerging testing strategies include the use of nasal swab or salivary samples rather than nasopharyngeal swabs. In addition, emerging point-of-care PCR testing will provide results more immediately instead of the typical 24-hour or more wait for laboratory-based PCR testing.
Another emerging strategy is point-of-care antigen testing, which assesses for the presence of a viral protein. With this method, up to 50 tests in one hour can be performed and can selectively identify any positive results without having to rerun the tests (as is typical for other types of bulk batch testing). Point-of-care antigen testing currently has relatively low sensitivity of around 70% to 90%, meaning it could miss some positive cases, but the sensitivity has been improving rapidly. On the other hand, its specificity is essentially 100%, meaning that the test should not produce false-positive results. Point-of-care antigen testing costs less that typical lab-based PCR testing. Because such testing may allow a combination of increased testing frequency combined with rapid speed of reporting, this may provide a benefit for surveillance testing that outweighs high sensitivity tests that are coupled with delayed (for example, more than 48 hours) reporting.[13]
Serology testing, either using IgG or IgM antibodies, has not been sufficiently validated to warrant its use for diagnostic testing purposes. Antibody testing may be considered to screen for possible previous exposure to SARS-CoV-2, but should not be used as the sole modality to determine potentially infected individuals.
Diagnostic testing refers to either PCR or point-of-care antigen testing to confirm or negate infection with COVID-19.
Surveillance testing is used to track patterns of spread in a community setting. Typically, a percentage of the population, or the entire population of a defined group, is tested without regard to whether the individual is symptomatic or may be engaged in high contact risk behavior. Surveillance testing may be used to help mitigate risk of an outbreak due to the sport activity. Repeat surveillance testing of someone who previously tested positive for the virus should not need to be performed; however, these individuals should continue to follow all risk mitigation strategies. Testing should be performed for new COVID-19 symptoms. This is an evolving area of research, and recommendations may need to be adjusted as new information arises about the definitive possibility of reinfection.
Diagnostic testing in athletics may be considered a combination of surveillance testing, testing individuals/groups engaged in high-risk exposure, and testing individuals with suspected COVID-19 infection. At present, scientific studies do not provide clear guidance on the following:
- Test sensitivity in asymptomatic people.
- Prediction rules for estimating the pretest probability of infection for asymptomatic individuals to allow calculation of post-test probabilities after positive or negative results.
- Thresholds for ruling out infection for a variety of clinical situations, including sport. Therefore, the testing strategies for asymptomatic athletes noted below are based on consensus recommendations and are subject to change as more data emerge.[14]
For the purposes of this document, based on current evidence and standards, PCR is the standard testing method for both baseline and ongoing surveillance testing. Testing strategies are always contingent on the availability of ample testing supplies, laboratory capacity, efficient turnaround time and convenient access to testing. If PCR testing in a community is prioritized for symptomatic individuals, if PCR supplies/turnaround time are compromised, or as testing technology evolves, alternative strategies may need to be considered.
Sport Classification Update
The categorization of sport risk was previously noted in the Action Plan document and is based on consensus from the NCAA COVID-19 Advisory Panel and the AMSSM COVID-19 Working Group and on the probability and significance of respiratory droplet spread during vigorous exercise when physical distancing and masking are not applied or are not possible. Importantly, the sport classification refers to sport-specific training and competition and not cross-training or other aspects of training. For example, swimming is a low contact risk sport, but dry land training activities such as trampoline, stretching, and tumbling may be associated with higher risk activity if risk-mitigating strategies noted above are not in place.
The risk assessment has now been updated below to include all NCAA-sponsored sports, including both winter and spring sports. Importantly, this risk assessment differs from the National Federation of State High School Associations and the United States Olympic and Paralympic Committee and also may differ from state/local risk categorization guidance.
- Low contact risk: bowling, diving, equestrian, fencing, golf, rifle, skiing, swimming, tennis, track and field.
- Medium contact risk: acrobatics and tumbling, baseball, beach volleyball, cross country*, gymnastics, softball, triathlon*.
- High contact risk: basketball, field hockey, football, ice hockey, lacrosse, rowing, rugby, soccer, squash, volleyball, water polo, wrestling.
* The level of risk in cross country, track and field and triathlon are dependent upon the student-athlete’s proximity to other unmasked individuals. For example, the start or finish of a race may involve a group of athletes who are breathing heavily in a group space with a breakdown in physical distancing.
Low Contact Risk and Medium Contact Risk Sports
If a team in a low contact risk or medium contact risk sport can successfully implement physical distancing and universal masking practices during all sport activities, then the risk of potential spread related to those sports will decrease. This becomes an important consideration as schools evaluate risks related to competition with other member schools and make decisions about how to employ testing resources and strategies. In any low contact risk or medium contact risk sport or other scenario where appropriate physical distancing and universal masking practices cannot always be maintained, schools should consider necessary testing strategies and protocols to mitigate community spread of COVID-19. Testing protocols should address student-athletes and all “inner bubble” personnel including coaches, medical staff, officials and other essential personnel who are at high risk of exposure. Two examples of possible testing protocols are provided below:
- Scenarios Presenting Medium Contact Risk:
- Diagnostic testing upon arrival to campus.
- During summer athletic activities and out-of-season athletic activities: surveillance PCR testing, for example, testing 25%-50% of athletes and “inner bubble” personnel every two weeks if physical distancing, masking and other protective features are not maintained, plus additional testing for symptomatic and high-contact risk individuals.
- During in-season (preseason, regular season and postseason): surveillance PCR testing, for example, 25%-50% of athletes and “inner bubble” personnel every two weeks if physical distancing, masking and other protective features are not maintained, plus additional testing for symptomatic and high contact risk individuals.
- Symptomatic testing and high-contact risk testing as appropriate.
- Scenarios Presenting Low Contact Risk:
- Diagnostic testing upon arrival to campus.
- During summer athletic activities and out-of-season athletic activities: surveillance testing in conjunction with a university plan for all students, plus additional testing for symptomatic and high contact risk individuals.
- During in-season (preseason, regular season, postseason): symptomatic testing and high contact risk testing thereafter.
High Contact Risk Sports
Because it is highly unlikely that physical distancing and universal masking can always be maintained during practice and competition in high contact risk sports, schools should consider necessary testing strategies and protocols to mitigate community spread of COVID-19. Testing protocols should address student-athletes, plus all “inner bubble” personnel (coaches, medical staff, officials and other essential personnel) for whom physical distancing, masking and other protective features are not maintained.
For high contact risk sports teams returning to campus and engaging in voluntary and required summer athletic activities and out-of-season athletic activities, schools should contemplate initial testing upon return. Further, schools should consider surveillance testing every two weeks thereafter during voluntary and required summer athletic activities, as well as out-of-season athletic activities for all student-athletes and “inner bubble” personnel if physical distancing, masking and other protective measures are not maintained. For high contact risk sports that are in-season (preseason, regular season, postseason), weekly surveillance testing should be performed for student-athletes, plus “inner bubble” personnel for whom physical distancing, masking and other protective features are not maintained. (See Table 1 below for graphic summary.)
Table 1. Testing Strategy Considerations for High Contact Risk Sports
|
Arrival on Campus
|
All athletes and “inner bubble” personnel are tested.
|
|
Summer Athletic Activities (Voluntary)
|
Surveillance PCR testing, for example, 25%-50% of athletes and “inner bubble” personnel every two weeks if physical distancing, masking and other protective features are not maintained*, plus additional testing for symptomatic and high contact risk individuals |
|
Summer Athletic Activities (Required)
|
Surveillance PCR testing, for example, testing 25%-50% of athletes and “inner bubble” personnel every two weeks if physical distancing, masking and other protective features are not maintained*, plus additional testing for symptomatic and high contact risk individuals. |
|
In-Season (Pre-Season, Regular Season, Post-Season)
|
Weekly PCR testing** of all athletes, plus “inner bubble” personnel for whom physical distancing, masking and other protective features are not maintained; additional testing for symptomatic and high contact risk individuals. |
|
Out-of-Season Athletic Activities
|
Surveillance PCR testing, for example, 25%-50% of athletes and “inner bubble” personnel every two weeks if physical distancing, masking and other protective features are not maintained*, plus additional testing for symptomatic and high contact risk individuals. |
* Those unable to fully implement appropriate sanitization, physical distancing and masking in all activities.
** Competition testing may account for the weekly testing
Updated Competition Considerations
With respect to competition with other schools, athletics departments should consider how best to secure reasonable assurance that the same risks have been adequately considered and addressed by the other team. Schools should consider how to share testing results and related safety assurances to opposing teams before the start of an event in a manner consistent with applicable health information and education privacy laws. Further, in conjunction with local public health officials and contact tracers, schools should have in place a mechanism for notifying other schools should an athlete from one team test positive within 48 hours after competition with another team.
Pre-Competition Testing
School and conferences should contemplate pre-competition testing protocols that include all high contact risk student-athletes and officials, plus “inner bubble” personnel for whom physical distancing, masking and other protective features are not maintained. Schools should plan to secure the resources necessary to both perform the tests and to manage the details related to any positive results. In addition to general health and safety risks related to potential disease spread, the complexities related to pre-competition testing should encourage schools to limit the number of “inner bubble” individuals involved with each competition.
For all high contact risk sports, protocols should be contemplated that include testing of student-athletes within 72 hours of competition for football and within 72 hours of the first of the week’s set of games for other high contact risk sports. Officials in football and basketball, due to their close contact with athletes, should also be tested weekly. Athletes must continue all infection risk mitigation behaviors after testing.
If PCR testing cannot be performed within 72 hours of competition, then the competition should be postponed or canceled, or an alternative plan for testing should be developed and agreed upon. This should include consultation with conference and local health officials before implementation. If an alternative, agreed upon testing strategy results in a lower sensitivity test result, repeat testing before competition should be considered to mitigate false negative results.
Clinical-Based Testing and Isolation
In addition to routine surveillance and pre-competition testing, schools and conferences should contemplate protocols that include clinical evaluation for student-athletes and/or other athletics personnel who develop COVID-19 symptoms after pre-competition testing, including testing for the presence of the virus. If a student-athlete or staff member becomes symptomatic between testing and competition, protocols should be considered that include isolating the student-athlete or staff member until repeat results are available, in each case in a manner consistent with applicable state, local and institutional recommendations.
Game Officials
Officials and referees may operate in proximity to student-athletes and school personnel during or as part of competition events. As a result, they may create risk for these individuals, and may also be at risk for contracting the disease from student-athletes. Athletics departments should consider how best to plan for and address these additional risks. For example, schools should consider the implementation of appropriate distancing and masking practices, as well as the use of electronic whistles, and should consider how best to ensure that officials are aware of any other competition-specific practices or expectations that will be implemented for risk mitigation purposes (for example, teams not swapping benches between periods). Note: Officials and referees in football and basketball would be considered part of the “inner bubble” of personnel deemed essential to the conduct of competition for purposes of pre-competition testing as noted above. Additional considerations also may need to be given to logistical issues, such as locker room and hospitality facilities typically used by officials and referees, and ingress and egress strategies to competition venues.
Universal Masking
As part of agreed-upon competition protocols, schools and conferences should contemplate universal masking for all coaches and other personnel who are present at the event. This can help prevent the unwitting spread of infection to others with whom they may have close contact, especially when talking at a close physical distance as is so common on the sidelines or bench area. Similarly, because wearing a mask/cloth face covering/face shield will not adequately protect a coach from infection by an infectious athlete, schools and conferences should contemplate a policy of universal masking for all student-athletes when they are not playing and when they move from the court/field to the sidelines for timeouts or between-period strategy discussions.
Team Travel
Public travel poses logistical challenges related to potential exposure and appropriate risk mitigation. Schools should continue to evaluate the current data regarding risks related to commercial plane and other travel, and travel protocols should be considered that include physical distancing, as possible, and universal masking for all individuals traveling with others by private car, van, chartered bus or chartered plane. Schools should also plan for proper communication of all travel rules, protocols and expectations to everyone in the travel party. When feasible, schools should aim to travel and play the same day to avoid overnight stays. For overnight stays or same-day travel, prepackaged meals or room service should be considered. If restaurant dining is the only option, consider take-out food or outdoor eating as preferable alternatives.
Updated Contact Tracing Considerations
Effective contact tracing is critical in breaking the chain of transmission and limiting the spread of infection for infectious diseases such as COVID-19. However, there is no federal oversight of contact tracing programs, and the number of contact tracers in this country is currently inadequate to effectively manage disease spread among individuals and groups of people with high contact risk exposure. As a result, athletics departments, in consultation with institutional leadership, should consider evaluating the availability of, and accessibility to, local contact tracing resources. Where the availability of local contact tracing resources is identified as inadequate, schools should consider the need for and benefit of training on-site personnel through accepted courses such as the Coursera class. Staff who complete formal training in contact tracing can be an invaluable resource with respect to institutional risk-management efforts and resources.
Considerations After a Positive Test Result
When an athlete tests positive for COVID-19, local public health officials must be notified, and contact tracing protocols must be put in place. All individuals with a high risk of exposure should be placed in quarantine for 14 days as per CDC guidance. This includes members of opposing teams after competition. The difficulty is defining individuals with a high risk of exposure, and in some cases, this could mean an entire team (or teams). The CDC defines a close contact requiring quarantine as:[15]
- An individual who was within 6 feet of someone with COVID-19 for at least 15 minutes.
- An individual who provided care at home to someone who is sick with COVID-19.
- An individual who had direct physical contact with the person (touched, hugged, or kissed them).
- An individual who shared eating or drinking utensils.
- An individual who was sneezed or coughed on by an infected individual or who somehow was touched by respiratory droplets from an infected individual.
Considerations Related to the Discontinuation of Athletics
At the time of this writing, the rate of spread of COVID-19 has been increasing in many regions of the country. Because of this increase, it is possible that sports, especially high contact risk sports, may not be practiced safely in some areas. In conjunction with public health officials, schools should consider pausing or discontinuing athletics activities when local circumstances warrant such consideration. Some examples of such local circumstances that might trigger a conversation with local public health officials include:
- A lack of ability to isolate new positive cases or quarantine high contact risk cases on campus.
- Unavailability or inability to perform symptomatic, surveillance and pre-competition testing when warranted and as per recommendations in this document.
- Campuswide or local community test rates that are considered unsafe by local public health officials.
- Inability to perform adequate contact tracing consistent with governmental requirements or recommendations.
- Local public health officials stating that there is an inability for the hospital infrastructure to accommodate a surge in hospitalizations related to COVID-19.
